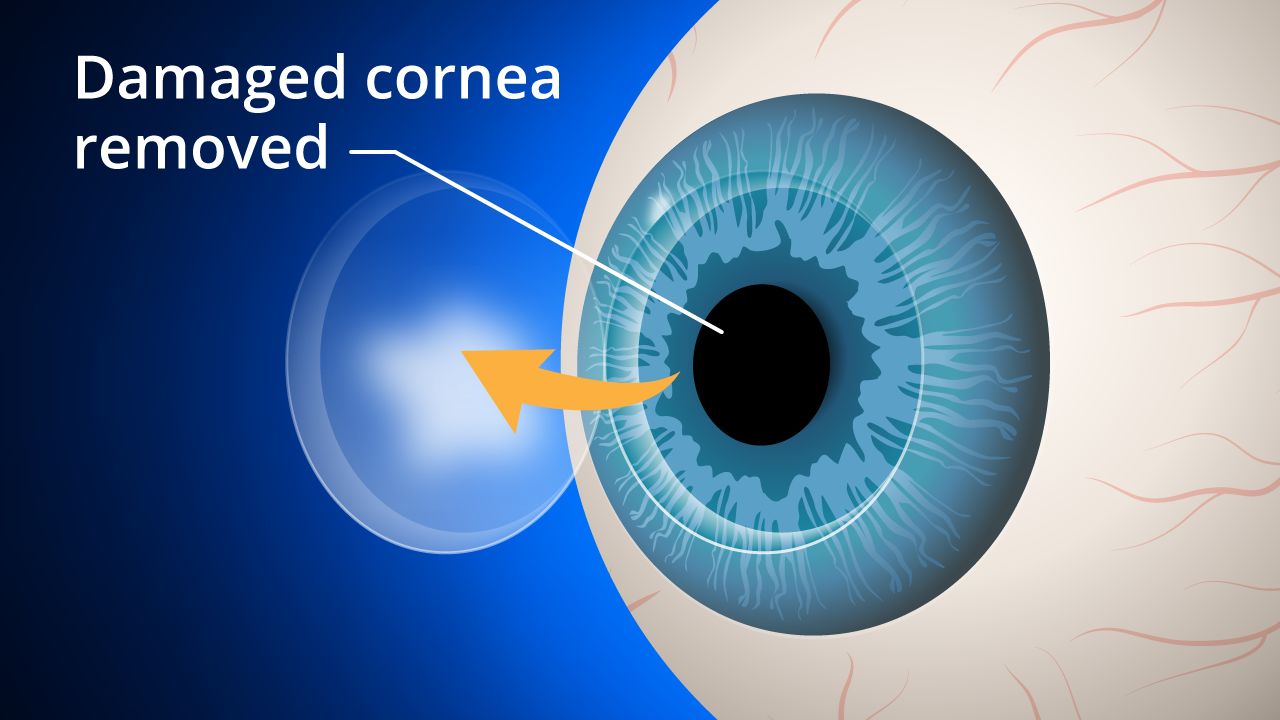
A cornea transplant, also known as a keratoplasty, is a surgical procedure that involves the replacement of the damaged or diseased cornea with a healthy cornea from a donor. The cornea is the transparent, dome-shaped layer at the front of the eye that helps focus light into the eye. If the cornea is damaged or diseased, it can cause vision problems, including blurred vision, sensitivity to light, and distortion.
Cornea transplant is one of the most common and successful types of organ transplant. According to the Eye Bank Association of America, there were over 85,000 corneal transplants performed in the United States in 2020. The procedure is typically performed by an ophthalmologist, a medical doctor who specializes in eye care.
There are several reasons why someone may need a cornea transplant. The most common reason is a condition called keratoconus, which causes the cornea to become thin and bulge outward, resulting in distorted vision. Other reasons for a cornea transplant may include:
- Fuchs' dystrophy: a condition that causes the inner layer of the cornea to break down, leading to swelling and cloudy vision
- Corneal scarring: caused by an injury or infection that damages the cornea
- Corneal ulcers: a serious infection of the cornea that can cause vision loss if not treated promptly
- Other rare conditions that affect the cornea, such as corneal degeneration or corneal ectasia
There are several types of cornea transplant, and the choice of procedure will depend on the specific needs of the patient. The most common types of cornea transplant include:
- Penetrating Keratoplasty (PK): In this procedure, the entire damaged cornea is replaced with a healthy donor cornea. The surgeon makes a circular incision in the patient's cornea and removes the damaged tissue, replacing it with a similarly sized donor cornea. The donor cornea is held in place with tiny stitches, which are removed at a later time.
- Deep Anterior Lamellar Keratoplasty (DALK): In this procedure, only the outer layer of the cornea is replaced, leaving the patient's own inner layer intact. This is a good option for patients with conditions that affect the outer layer of the cornea, such as keratoconus.
- Endothelial Keratoplasty (EK): In this procedure, only the innermost layer of the cornea is replaced. This is a good option for patients with conditions that affect the endothelial layer of the cornea, such as Fuchs' dystrophy.
Preparing for Cornea Transplant
Before a cornea transplant, the patient will undergo a thorough eye examination to determine the cause of their vision problems and to ensure that they are a good candidate for the procedure. The patient's medical history will also be reviewed, and any medications they are taking will be evaluated to determine if they need to be adjusted prior to surgery.
The patient will also need to arrange for a donor cornea to be available for their surgery. Donor corneas are typically obtained from eye banks, which collect and store corneas from deceased donors. The cornea must be carefully matched to the patient's eye, taking into account factors such as the size and shape of the eye.
The cornea transplant is typically performed under local anesthesia, which numbs the eye but allows the patient to remain awake during the procedure. The surgery usually takes about one to two hours to complete.
The surgeon will start by making a circular incision in the patient's cornea and removing the damaged tissue. They will then carefully insert the donor